The Color of Medicine?
Like many family medicine physicians, one of the reasons I chose my “specialty” was to serve the millions of Americans who feel ignored and abandoned by the medicine field. In medical school, I learned about biases and discrimination that minority populations were repeatedly subjected to. We were informed of these accounts to show us why certain populations may not trust physicians and hospitals and how changing the delivery of medicine from paternalistic relationships to shared decision-making models would improve those partnerships.
However, it was also my medical education that taught how due to genetics, certain races had higher risks of heart disease, needed different calculations for determining kidney functioning, altered pulmonary function thresholds, and had different composition of muscle fibers. I was taught that these were non-modifiable and just the way it was — you can’t deny genetics. So imagine my bewilderment years later when I learned that many of these “facts” had foundations in certain individuals trying to prove “race inferiority” and to allow African Americans to receive inferior treatment compared to their Caucasian counterparts.
Blog continued Heading link

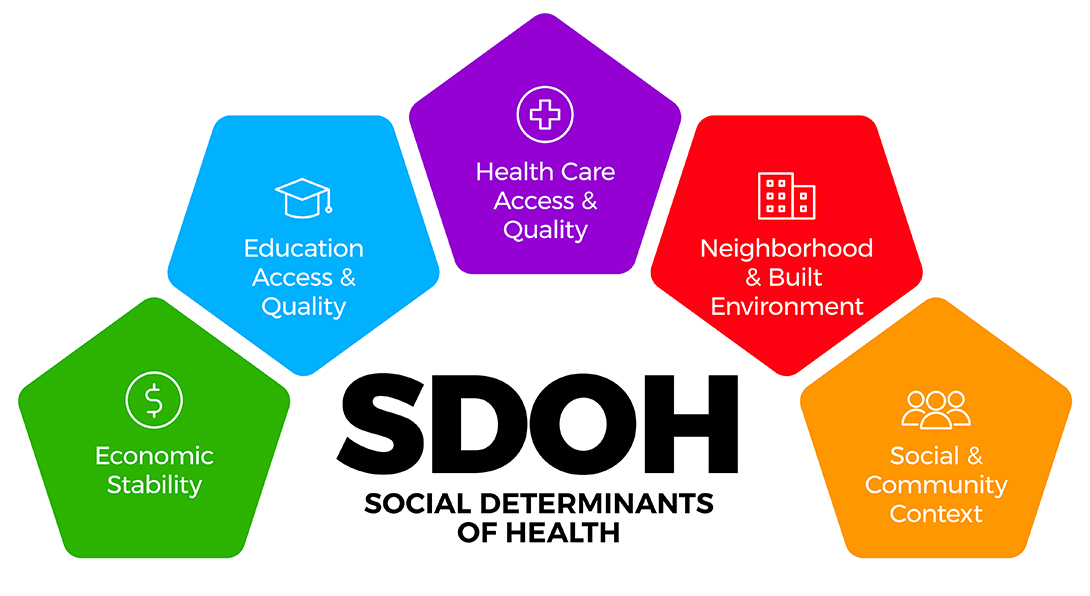
Social Determinants of Health
I had learned about social determinants of health (SDOH) but not until late in my medical training did I start to understand that these SDOH were oftentimes just symptoms of oppression that millions of Americans of color have been subjected to for years. After years of trying to make my patients healthier with lifestyle changes and medication, I now see that I must do more to truly serve my patients. I need to not just think of individual encounters in our family medicine office, but how to make my entire community healthier by learning how to help right previous injustices.
Currently I am in the research phase of this undertaking — learning the history of those inequities. The latest book I finished, “The Color of Law” by Richard Rothstein (recommended by one of our previous residents, who went on to a community medicine fellowship in California), was one of the biggest eye openers yet. This book is about how the federal, state and local government segregated our country with zoning, lending practices, tax laws, labor union regulation, and failure to enforce fair law enforcement policies. (Many of the statistics in the following paragraphs are cited from “The Color of Law).”
Unfair Banking Practices
When I learned of the New Deal in high school, I learned only positives from my high school textbook. I learned how the New Deal turned this country around from the Depression with public works, assistance with housing, creating infrastructure, etc.
I was not taught how the federal government refused to insure bank loans to African Americans until the 1960’s, which included blatant refusal in the 1910’s-1930’s and more “veiled” practices like redlining. Without having access to loans, African Americans were forced into contract sales that had inflated monthly payments and, if one payment was missed, the tenant was kicked out without any ownership/equity in the house. Policies like these forced African Americans to work multiple jobs (many of which were entry level due to employment discrimination) and have multiple subtenants to help pay the rent, while resulting in less time to provide maintenance to their house. These practices of contract sales, block-busting and redlining were all formed to segregate certain races and socioeconomic classes. Single family housing was restricted to only white families, and many white-only neighborhoods refused to allow multi-family houses or apartments. It was estimated in 1954 by the Federal Housing Agency (FHA) that African Americans were overcrowded four times the rates of Caucasians.
Quote Heading link
I need to not just think of individual encounters in our family medicine office but how to make my entire community healthier by learning how to help right previous injustices.
| Department of Family & Community Medicine
Blog continued Part 2 Heading link
Housing and Neighborhood Inequity
What has resulted from many of these previous practices is less African American families were allowed to build household wealth due to inability to build/buy a house when income: house price ratio was much higher (home equity is the main source of wealth for middle-class Americans) in the 1930s-1980s. The median white household is currently $134,00 while black household wealth is $11,000. Not being able to borrow from your home equity prevents families from covering emergency medical bills, enduring periods of joblessness, or retirement. One of the main factors that determines a generation’s wealth is the wealth of the generation before. Thus, this cycle will continue to widen unless we intervene.
Currently, young African Americans are now ten times more likely to live in poor neighborhoods than Caucasian youths (66 % vs 6%). Oftentimes in more urban neighborhoods with higher levels of families below the poverty line, there is less access to fresh food, schools are overcrowded, there is stress from increased gun violence, there are fewer primary care providers, and there are increased airborne pollutants as industry is usually closer to these neighborhoods.
Family Medicine Physicians as Advocates
So with all these barriers to basic needs, how can we as family medicine physicians help our patients get healthier? Of course, I will continue to treat my patients’ high blood pressure, recommend age-appropriate cancer screenings, and treat each patient with respect. However, electing local city and state politicians to fix local zoning ordinances, fighting for historically accurate education in our school districts, pushing for equity and bias-free employment at our place of work are also our obligations. We as family physicians need to be advocates for our patients, not only in our office but also in our communities.