The Asuthkar Cancer Lab

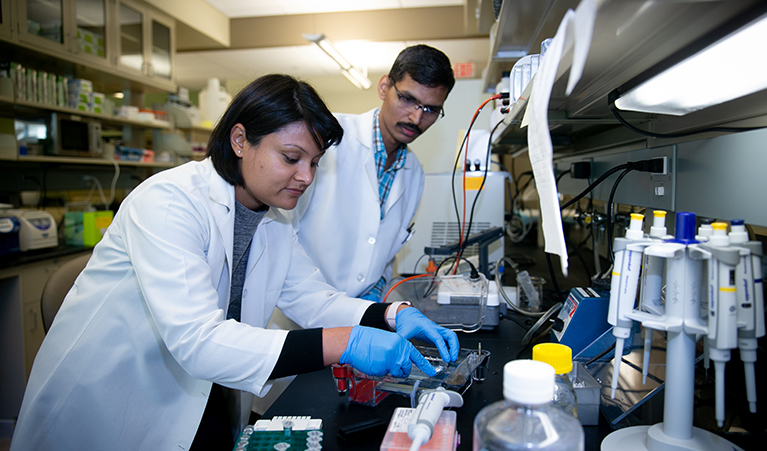
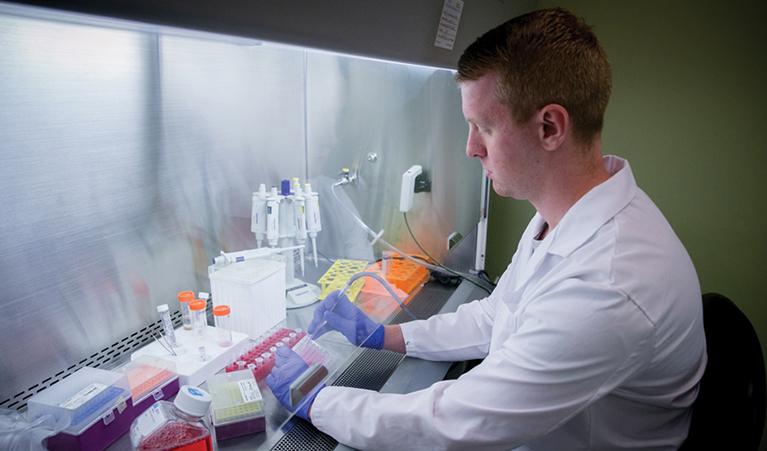
Swapna Asuthkar’s lab investigates the molecular mechanisms of cancer progression and identifies novel targets for therapeutic intervention.
Lab Focus Areas Heading link
Her research primarily involves the use of molecular biology, biochemistry and biophysics techniques to study the underlying mechanisms of cancer, with a focus on cancer signaling pathways that are involved in migration, invasion and metastasis.
Her lab also focuses on understanding the protein-protein interactions that drive cancer progression. Studies look at how these interactions can be targeted to inhibit cancer growth. The lab also investigates the combination of chemotherapy and radiotherapy to target these mechanisms and develop new therapeutic strategies for cancer treatment.
Overall, the goal of her research is to better understand the molecular mechanisms of cancer and identify new targets for drug development, with the ultimate goal of improving patient outcomes and enhancing cancer treatment.
Meet the Lab Director Heading link
Collaborators Heading link
Primary Collaborators
Rajeev Vibhakar, MD, PhD, Univ. of Colorado
Sujatha Venkataraman, PhD, Univ. of Colorado
Andrew J Tsung, MD, INI
Kiran K Velpula, PhD, UICOMP
Sarah E. Martin, MD, OSF
Justin Lathia, PhD, Cleveland Clinic
Francesca Perut, PhD, Istituto Ortopedico Rizzoli, Italy
Dr. Rambabu Gundla, Advisory Member, Ciencia Labs LLP, India
Dr. Sabitha Yadam, Ciencia Labs LLP, India
Secondary Collaborators
Eleonora Zakharian, PhD, UIC Peoria
Dr. Timothy E. Koeltzow, Dept. of Psychology, Bradley University
Gail S. Prins, PhD, UIC Chicago
Michael X. Zhu, PhD, Univ. of Texas
Hehuang “David” Xie, PhD, Virginia Tech
Alexander Sobolevsky, PhD, Columbia Univ.
Baskaran Thyagarajan, PhD, Univ. of Wyoming
Vander Don Griend, PhD, UIC Chicago
Exploring the Role of Immune Checkpoint Molecules in Cancer Progression and Metastasis Heading link
B7-H3, also known as CD276, is an immune checkpoint protein that has been shown to be overexpressed in a variety of human cancers, including medulloblastoma and lung cancer. Studies have linked high levels of B7-H3 with poor prognosis. Our lab, is dedicated to understanding the role of this protein in cancer progression and mestasis, and identifying new strategies for treatment.
The role B7-H3 plays in cancer may be more significant than previously thought.
Our research has shown that B7-H3 plays a significant role in host cell interaction, cancer progression, angiogenesis, and metastasis. We have found that high levels of B7-H3 expression correlate with the activation of the PI3K/Akt signaling pathway, which promotes cancer cell proliferation, survival, and angiogenesis. Additionally, we have investigated the role of B7-H3 in medulloblastoma progression and found that high B7-H3 expression is associated with a higher risk of recurrence and poorer overall survival. Furthermore, B7-H3 plays a critical role in the regulation of the tumor microenvironment by promoting the recruitment and activation of immune cells that contribute to tumor growth, progression, and metastasis. Our research also showed that B7-H3 is expressed in exosomes, which do not require receptors for cell-cell contact, indicating its role in cancer may be more significant than previously thought.
What we hope to accomplish
Our lab aims to further understand the regulatory factors that affect B7-H3 expression and determine its oncogenic properties in order to develop new treatments for cancer patients. Targeting B7-H3 through immune checkpoint inhibition may be a promising strategy for treating medulloblastoma and other cancers. We are committed to advancing our understanding of this important protein and developing new treatments to improve the prognosis for cancer patients.
Uncovering the Epigenetic Secrets of Medulloblastoma: Targeting Key Protein Markers for Improved Treatment Outcomes Heading link
The research focus of Asuthkar’s lab is the identification of key epigenetic markers that contribute to the development and progression of Group 3 medulloblastoma (MB) using next-generation sequencing data.
The goal is to understand how these markers contribute to the disease and develop targeted therapies that can improve treatment outcomes, especially in cases where radiation therapy (RT) is ineffective due to the development of radioresistance (RR).
Epigenetic markers, SMYD3 and EZH2
The lab has identified specific epigenetic markers, such as SMYD3 and EZH2, that can sensitize cancer cells to radiation therapy and promote the development of MB by increasing the expression of cell cycle proteins. Targeting these markers, like SMYD3, with small molecule inhibitors could be a promising strategy for treating this type of cancer.
What we hope to accomplish
The lab’s research aims to improve the quality of life and survival of cancer patients by identifying key protein markers and developing targeted therapies against them, with a specific focus on Group 3 medulloblastoma, a highly aggressive brain cancer with limited treatment options. The lab is also actively investigating the use of epigenetic modifiers as adjuvants to standard cancer therapies to combat RR.
Unlocking the Secrets of TRPM8: A Potential Key to Prostate Cancer Treatment and Beyond Heading link

The seminal findings of Asuthkar’s lab research include identifying that the Transient receptor potential melastatin 8 (TRPM8) is a tumor suppressor and a key element of the orphan pathway for non-genomic testosterone actions. TRPM8 is a cold-sensing and Ca2+ permeable channel protein. Oscillations in intracellular Ca2+ levels stimulate cell proliferation and survival while sustained cytosolic Ca2+ concentrations promote apoptosis.
What we hope to accomplish in the long term
Asuthkar’s long-term goal is to achieve therapeutic benefit by inhibiting the desensitization mechanism of TRPM8 channel activation in prostate cancer, subsequently causing apoptotic cell death. In light of these observations, her studies support a strategy for rescuing plasma membrane levels of TRPM8 as a new therapeutic application for prostate cancer.
The research also suggests that TRPM8 is a rapid testosterone signaling receptor with implications in the regulation of dimorphic sexual and social behaviors, meaning that TRPM8 plays a role in the regulation of behaviors that are unique to males and females, such as sexual behavior and social interactions. However, it’s important to note that these findings are based on laboratory studies, and their applicability to human patients is still unknown.
Further studies and clinical trials are needed to confirm these findings and to determine the potential use of TRPM8 as a therapeutic target for prostate cancer, as well as to determine the extent of TRPM8’s role in regulating dimorphic sexual and social behaviors.